On This Page[Hide][Show]
Post-exertional malaise is a common symptom experienced by individuals with chronic illnesses, often leading to significant limitations in their ability to work and engage in daily activities. If you are considering filing a long-term disability claim due to post-exertional malaise, it’s crucial to understand the specific requirements and documentation needed to support your claim. In this blog post, we will provide a comprehensive overview of long-term disability claims for post-exertional malaise, equipping you with the knowledge to approach the claims process effectively.
Understanding Post-Exertional Malaise (PEM)
Definition and Symptoms
Post-exertional malaise (PEM), sometimes called post-exertional symptom exacerbation (PESE), is when your symptoms worsen, or you develop new symptoms after physical or mental activity that would not have caused the same reaction in a healthy individual. It is a defining characteristic of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
The symptoms can include extreme fatigue, pain, cognitive dysfunction, dizziness, and flu-like symptoms. Individuals may experience a delayed response, with symptoms peaking 12 to 48 hours after the exertion.
Impact on Daily Life
PEM significantly impairs an individual’s ability to carry out daily activities. Everyday activities like grocery shopping, laundry, or cooking can lead to prolonged exhaustion and increased pain. This creates a cycle of pushing beyond limits, experiencing PEM, and then requiring extended rest periods to recover, further reducing overall functionality and quality of life. The unpredictability of PEM can also lead to social isolation and an inability to maintain regular work schedules, often resulting in financial burdens and emotional distress.
Long-Term Disability Coverage
When it comes to dealing with long-term disability (LTD) claims for post-exertional malaise, understanding the coverage provided by your policy is essential. Reviewing your policy in detail will give you a clear understanding of what is included and excluded from your coverage.
Reviewing Your Policy
Reviewing your long-term disability policy involves carefully examining the terms and conditions outlined in the document. Look for details related to post-exertional malaise and understand how the policy defines and addresses this condition. Pay close attention to any non-medical requirements, limitations, waiting periods, and exclusions that may impact your claim.
Understanding Eligibility Criteria
Alongside reviewing your policy, understanding the medical eligibility criteria for long-term disability claims is crucial. Different insurance providers may have varying criteria for assessing post-exertional malaise and its impact on an individual’s ability to work. Familiarize yourself with the specific requirements related to this condition to determine whether you meet the criteria for filing a claim.
By delving into these aspects of long-term disability coverage, you can gain valuable insights into the coverage afforded by your policy and the criteria you must meet to receive benefits for post-exertional malaise. Understanding these details will help you navigate the long-term disability claim process effectively.
Filing a Long-Term Disability Claim for Post-Exertional Malaise
Navigating the complexities of filing a long-term disability claim for post-exertional malaise can be overwhelming, but with the proper guidance and knowledge, the process becomes more manageable. Three crucial aspects to consider when filing a long-term disability claim for PEM include gathering medical evidence, working with healthcare providers, and completing the necessary forms.
Gathering Medical Evidence
When filing a long-term disability claim for PEM, gathering comprehensive and compelling medical evidence is paramount. This evidence should clearly outline the impact of PEM on the individual’s ability to perform daily tasks, maintain employment, and engage in social activities. It’s essential to collect medical records, test results, and physician notes that explicitly articulate the limitations imposed by PEM.
Working with Healthcare Providers
Collaborating closely with healthcare providers is instrumental in substantiating a long-term disability claim for PEM. Physicians’ familiarity with the nuances of PEM can provide invaluable insights and documentation to support the claim. Establishing open communication with healthcare providers and ensuring they comprehend the specific challenges PEM poses can lead to more thorough and accurate medical assessments, improving the claim’s validity.
Completing the Necessary Forms
Completing the required forms is critical in the long-term disability claims process. Each form should be meticulously filled out, providing detailed accounts of the individual’s medical history, the impact of PEM on their daily life, and the professional opinions of healthcare providers. Thorough and accurate completion of these forms can significantly influence the outcome of the claim.
The Importance of Detail and Specificity
When dealing with long-term disability claims for post-exertional malaise, the importance of detail and specificity cannot be overstated. Proper documentation of PEM episodes and effective communication with insurers is crucial for ensuring that your disability claim accurately represents your condition.
Documenting PEM Episodes
It is essential to document each PEM episode you experience meticulously. This includes recording your symptoms’ onset, duration, and severity and any specific triggers or aggravating factors. Detailed documentation can provide concrete evidence of the impact of PEM on your daily life and functional abilities. Consider keeping a symptom journal or using a health-tracking app to capture this information effectively.
Communicating Effectively with Insurers
When communicating with insurers, clarity and specificity are essential. Clearly articulate the nature of PEM, its impact on your ability to work and function, and how it aligns with the criteria for long-term disability. Provide detailed records of medical appointments, test results, and healthcare provider assessments to support your claims effectively.
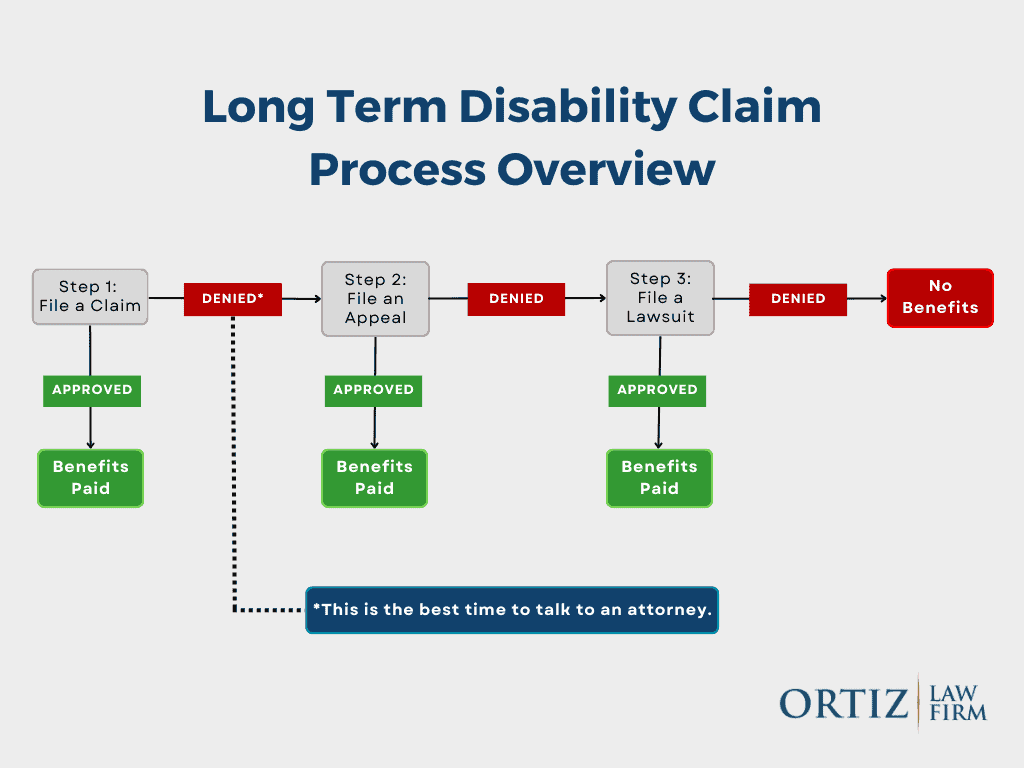
Appealing a Denied Claim
In case of a denied long-term disability claim for post-exertional malaise, it’s critical to understand the reasons for denial, gather additional evidence, and seek legal assistance if necessary. Understanding the reasons for denial can shed light on what aspects must be addressed on appeal or where additional information is required.

Understanding the Reasons for Denial
Upon receiving a denial, the first step is to review the reasons provided by the insurance company. Common reasons for denial may include insufficient medical evidence, failure to meet the definition of disability according to the policy, or missed deadlines in the claims process. Understanding these reasons will clarify the specific areas that need to be addressed in the appeal.
Gathering Additional Evidence
Following the denial, the next step involves gathering additional evidence to support the claim. This may include obtaining further medical documentation, test results, or physician statements that strengthen the case for disability due to post-exertional malaise. Additionally, gathering testimonies from colleagues, supervisors, or friends regarding the condition’s impact on daily functioning can provide valuable supplementary evidence.
FREE RESOURCE: Appeal a Long-Term Disability Denial with our Disability Insurance Appeal Guide
Seeking Legal Assistance If Necessary
Should the appeals process become too complex or overwhelming, seeking legal assistance from an attorney experienced in disability claims can be beneficial. Legal professionals can help claimants navigate the appeals process, ensuring that all necessary documentation and evidence are presented effectively. Moreover, they can advocate for the claimant’s rights and represent their interests in negotiations with the insurance company.
It’s crucial to approach the appeal process systematically, addressing the reasons for denial, bolstering the claim with additional evidence, and seeking legal support if needed. By following these steps, claimants increase their chances of successfully appealing a denied long-term disability claim for post-exertional malaise.
Schedule a Free Case Review
Navigating the claims process can be daunting, but claimants can position themselves for a favorable outcome. It’s imperative to gather thorough medical documentation, adhere to deadlines, and, if necessary, seek the assistance of legal experts with experience in disability claims. By taking these proactive steps, individuals can improve their chances of securing the long-term disability benefits they rightfully deserve.
We have a “No Recovery, Zero Fee Guarantee.” This means our clients only pay a fee when disability benefits are recovered.

However, even well-supported claims are sometimes denied. If your claim has been rejected, you should speak with an experienced professional to better understand the strengths and weaknesses of your claim and your appeal rights. The Ortiz Law Firm is a national disability law firm located in Pensacola, Florida. Under the leadership of disability attorney Nick Ortiz, we help individuals across the country obtain the disability benefits they deserve. Don’t waste another day fighting with your insurance carrier – contact us online or call (888) 321-8131 to schedule a free case review.
Sources
- U.S. Centers for Disease Control and Prevention. “Strategies to Prevent Worsening of Symptoms” Retrieved from (https://www.cdc.gov/me-cfs/hcp/clinical-care/treating-the-most-disruptive-symptoms-first-and-preventing-worsening-of-symptoms.html) Accessed on January 12, 2024.

