On This Page[Hide][Show]
If you’re navigating the world of long-term disability insurance claims due to degenerative disc disease, you’re not alone. This comprehensive guide provides the essential information you need to understand the process and maximize your chances of a successful claim.
What Is Degenerative Disc Disease?
Degenerative disc disease (DDD) is perhaps the most common impairment for which people apply for disability benefits, aside from uncontrolled high blood pressure and diabetes (and the accompanying neuropathy that generally goes with diabetes). Despite the many disability claims for this impairment, it is not easy to be approved for disability for degenerative disc disease.
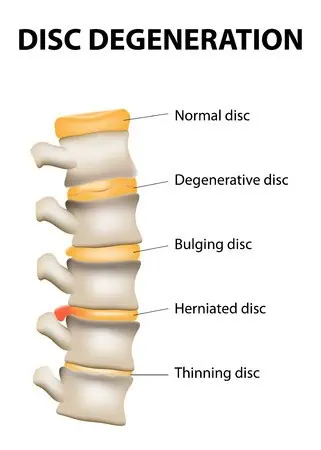
Intervertebral disc degeneration is one of the most common mechanical causes of low back pain. It occurs when the usually rubbery discs between the vertebrae of the spine lose integrity as a normal aging process. In a healthy back, intervertebral discs provide height between the spinal vertebrae and allow bending, flexion, and torsion. As the discs deteriorate, they lose their cushioning ability.
Degenerative disc disease is a common condition that affects all age groups – young to middle-aged men and women equally. Changes in the mechanical properties of the disc lead to degenerative arthritis in the intervertebral joints and osteophytes and may narrow the intervertebral foramen or the spinal canal.
Diagnosis of Degenerative Disc Disease
Upon physical examination, patients with DDD typically exhibit the following findings: limitation of movement, problems with balance, pain, loss of reflexes in the extremities, muscle weakness, loss of sensation, or other signs of neurological damage. For accurate diagnosis, combining clinical examination and sophisticated technology is often necessary.
A medical diagnosis (“clinical diagnosis”) focuses on determining the underlying cause of a patient’s lower back or neck pain, nerve pain, or other symptoms. There are four steps to arriving at a clinical diagnosis for a pinched nerve or disc pain:
- Physical examination: Depending on the patient’s symptoms, a physical exam may include one or more of the following tests:
- Nerve function in certain parts of the leg or arm: This test involves tapping specific upper or lower extremities with a reflex hammer. If the patient has little or no reaction, that indicates a compressed nerve root in the spine.
- Muscle strength: To better understand whether a herniated disc compresses the spinal nerve root, the examining doctor may conduct a neurological exam to assess muscle strength. The doctor may also ask the patient to partially undress to view the patient’s muscles, particularly to determine if there is muscle atrophy, twitching, or abnormal movements.
- Pain with palpation or motion: Checking for pain with palpitation or motion can indicate what is generating pain. For example:
- Pain over the sacroiliac joint (at the very bottom of the spine) to palpation may indicate sacroiliac joint dysfunction.
- Pain with leg straightening can be indicative of a pinched nerve.
- Pain with pressure on the lower back may indicate pain due to a degenerative disc.
- Review of specific symptoms: A complete review of the patient’s symptoms includes the location of the pain, a description of how the pain feels (such as searing pain vs. a dull or achy pain), and whether certain activities, positions, or treatments make the pain feel better or worse.
- Review of medical history: A complete review of your medical history is essential to rule out (or identify) other possible conditions that may be causing the patient’s pain. The history includes information such as any recurring health problems, previous diagnoses, past treatments and surgeries, reactions to prior treatments, current medications, family history of illness, and any other health concerns.
- Diagnostic tests: After forming an opinion about the cause of the patient’s pain, a physician may order a diagnostic test to confirm the disc problem or to gain additional information, such as the location of a herniated disc and impinged nerve roots. Diagnostic tests may include:
- CT Scan: Computerized tomography scans (CT Scans for short) work like X-rays in that an X-ray beam is shot through the body, and a computer reformats the image into cross sections of the spine.
- MRI scan: Whereas an X-ray focuses on bony structures, magnetic resonance imaging (MRI) allows doctors a sensitive and accurate assessment of the surrounding spinal nerves and anatomy, indicating disc alignment, height, hydration, and configuration.
- If surgery for disc pain is under consideration, some physicians may recommend a discogram to try and confirm which disc is painful. In this test, radiographic dye is injected directly into the disc; if the injected dye recreates the usual pain, then it is believed that the patient is suffering from disc pain (degenerative disc disease). There is controversy regarding whether this is a valid test. Many doctors do not use discography except in rare situations.
Degenerative Disc Disease and Long-Term Disability Claims
Disability insurance companies know that many people suffer from degenerative disc disease, a natural part of the aging process in which the vertebral discs shrink. For most people, the pain is intermittent, and they go on working. This is one of the fundamental problems regarding impairments that involve pain: only the person experiencing the pain knows how bad the pain is and how much it impairs them.
For this reason, disability claims handlers give little consideration to complaints of pain. Insurance companies typically only grant disability benefits to those whose disc disease has progressed into severely impacted vertebrae that cause severe and chronic pain and the inability to sit or stand for extended periods, and the underlying medical condition can be proven by medical imaging. That is why medical records are critical when it comes to degenerative disc disease and long-term disability.
How Do Insurance Companies Evaluate Disability Claims for Degenerative Disc Disease?
When a disability examiner opens a newly assigned disability application and sees either degenerative disc disease, back pain, cervical spinal stenosis, lumbar spinal stenosis, or degenerative joint disease, the examiner typically looks for the following evidence:
- Medical records that indicate one of these diagnoses.
- Objective evidence of disc deterioration [X-ray reports, CT scans (sometimes called CAT scans), and MRI studies.]
A disability examiner is looking for clinical evidence of nerve root compression (such as positive findings on a straight leg raise test), arachnoiditis (with imaging showing thickening and swelling of nerve roots due to inflammation of the arachnoid, one of the membranes known as meninges that surround and protect the nerves of the central nervous system, including the brain and spinal cord), or stenosis (such as an MRI showing narrowing of the spinal column).
In addition, the examiner will want to see that your DDD in the neck or back severely impacts your ability to function, such as by limiting:
- The range of motion in your spine;
- Your ability to walk effectively and
- Your ability to sit, stand, kneel, walk, push/pull, squat, twist, turn, bend, stoop, lift and carry weight, and reach overhead.
The Significance of Medical Evidence in DDD Cases
Interpretations of imaging studies (where a doctor reads an X-ray film and gives an opinion on its meaning) are critical in long-term disability claims. These objective medical findings are the only purely objective evidence in a disability case involving spinal problems of the neck or back.
In other words, a physician can diagnose degenerative disc disease based on a patient’s symptoms and a physical examination, but imaging studies give objective medical support for a medical condition that is reasonably expected to produce pain. For this reason, disability claimants should submit radiology reports from X-rays, CT Scans, and MRIs whenever possible.
Disability examiners will also carefully review the claimant’s medical treatment notes. The examiner will be especially interested in whether the claimant has a decreased range of motion, reduced muscular strength (doctors use a five-point scale; for example, 5/5 right leg strength indicates full right leg strength while 1/5 indicates severely diminished right leg strength), poor gait, and positive straight leg raises.
Medical records from treatment with a physician, particularly an orthopedist, are essential in a disability claim. Getting regular medical treatment from a medical doctor (MD) or osteopath (DO) can help ensure that you have sufficient medical records to substantiate your long-term disability claim for a degenerative back condition.
To be approved for long-term disability benefits for degenerative disc disease, you will need a great deal of medical evidence to corroborate your allegations.
Legal Assistance for Your Degenerative Disc Disease Claim
If your degenerative disc disease is so severe that you are no longer able to work, you may very well be entitled to receive long-term disability benefits. Because of the complexities involved with proving that this disease disables you, it would be in your best interest to consult with an experienced long-term disability attorney. If your claim is not handled correctly, you may never receive the benefits you deserve.
An experienced long-term disability lawyer knows how to obtain all the proper documents and medical opinions to satisfy your burden of proof. Mr. Ortiz is an experienced LTD attorney. He and his firm will work with you and your medical team to maximize your benefits from the insurance company. Call (888) 321-8131 for a free case evaluation if your claim has been delayed, denied, or terminated.

